H E A L T H
“DIABESITY:” A MODERN PANDEMIC
______________________
A shift toward sugared foods and less physical activity has caused a steady rise in obesity and diabetes, leading to the greatest health crisis of our time
______________________
WORLD HEALTH IS IN A DOWNWARD spiral as diabetes and cardiovascular disease rates soar. According to the International Diabetes Federation, India (after China) is home to the second largest number of diabetics in the world: 61.3 million. By 2030, that number will almost double to an estimated 101.2 million. The American Diabetes Association counted 25.8 million children and adults (8.3 percent of the population) with the disease in 2011. Another 79 million Americans are prediabetic. The ADA’s 2012 fact sheet projects that one in three American adults will have diabetes in 2050. That is merely a sampling of the burgeoning facts and figures that tell a grim tale of a disease that seems to be on a march to take over the world.
What is diabetes?
Dr. Francine R. Kaufman, head of the Center for Endocrinology, Diabetes and Metabolism at Children’s Hospital Los Angeles, explains in her best-selling book Diabesity: The Obesity-Diabetes Epidemic that Threatens America [http://www.amazon.com/Diabesity-Obesity-Diabetes-Threatens-America-And-ebook/dp/B000FCJZIG], “Diabetes can devastate nearly every system of the body, but it all starts with the metabolism of glucose, a type of sugar. Glucose is what fuels our every move and our every thought. The glucose we need comes from the food we eat. But our body can’t use it without insulin, a hormone produced by the pancreas.”
Diabetes comes in two forms. In type 1, the immune system destroys the special cells in the pancreas, called beta cells, that are responsible for producing insulin. Dr. Kaufman explains, “Type 1 diabetes typically appears in childhood and progresses rapidly. Fortunately, type 1 is relatively rare. Ninety percent of people with diabetes have the other kind, which is known as type 2. In type 2 diabetes, the key problem is not that insulin is lacking; rather, the body’s cells don’t respond normally to it. As with type 1, the cells go hungry while, paradoxically, glucose accumulates in the blood.”
_________________________________________________
“IF WE COULD PREVENT OBESITY, TYPE 2 DIABETES WOULD BECOME RARE.”
Francine R. Kaufman, M.D., in Diabesity
_________________________________________________
Type 1 diabetes is treatable with insulin injections, but can’t be cured. Dr. Kaufman writes, “Type 2 is different, because it’s strongly associated with excess weight. Simply by maintaining a healthy weight, people can significantly cut their risk of developing this terrible disease. What’s more, they can even cure it at its early stages if they achieve and maintain a normal weight.”
This connection with weight is the key. A joint statement from the American Diabetes Association and the American Heart Association begins: “The steady gain in the prevalence of obesity over the last 25 years has affected our entire population—no racial or ethnic group, no region of the country, and no socioeconomic group has been spared. Perhaps most worrisome is the observation that the rise in the rate of obesity has been greatest in children and minorities, which suggests that future generations of Americans, and our fastest growing populations, may bear the ultimate burden of this condition.
“Overweight or obesity results in a wide range of elevated risk factors and many fatal and nonfatal conditions. Paradoxically, although we have witnessed decades in which heart disease and stroke have steadily declined and cancer mortality has at worse remained stable, the prevalence of diabetes has soared. The increase in diabetes can largely be attributed to weight gain, and it threatens the enormous advances in disease prevention we have seen.”
Fully 80 percent of people with diabetes are overweight or obese. Dr. Kaufman explains that experts became alarmed by the parallel increase in obesity and diabetes that became apparent in the 1990s and began referring to them as a single problem. They called it “diabesity.”
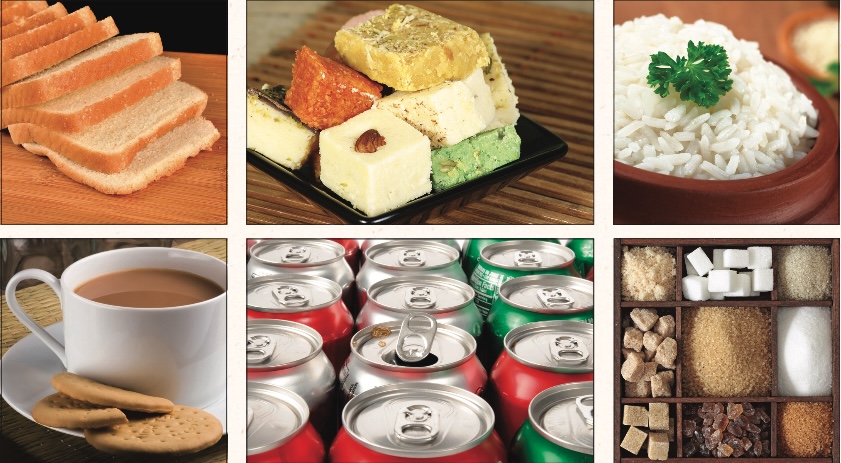
It’s all sugar: In tea and sweets, in white rice and flour products, no matter the form or color, glucose enters our bodies, spikes our blood sugar and puts on weight, time after time. The biggest culprit is soda.
• • • • • • • • • • • • • • • • • • • •
Excess weight around the midsection makes the disease more likely, but that’s not all. Dr. Kaufman elucidates, “Approximately one-third of obese adults, and perhaps as many overweight teenagers, have metabolic syndrome, which is also called syndrome X or insulin resistance syndrome.” Metabolic syndrome names a constellation of risk factors for diabetes and cardiovascular disease: high blood sugar, high waist circumference, high blood pressure, high levels of triglycerides and low levels of HDL, the good cholesterol.
The condition called prediabetes is commonly referred to more specifically by the term insulin resistance, describing the inability of cells to respond properly to insulin. This forms the cornerstone of type 2 diabetes, and it seems that it is caused directly by excess fat.
HINDUISM TODAY asked Dr. Vinaya Simha, an endocrinologist at the Mayo Clinic in Rochester, Minnesota, to elaborate: “Normally there is little to no fat in liver and muscle cells. With obesity, when the fat storing capacity of all fat cells is exhausted, then the muscle and liver cells also take up fat. Toxic products from the metabolism of triglycerides (the building blocks of fats) have been shown to interfere with insulin signaling in these cells, leading to insulin resistance. Obesity also imposes additional loads on the pancreatic beta cells.”
What is making us fat?
The simple answer: our food—specifically, the amount of sugar in foods and the quantity of refined starches most people are consuming as dietary staples.
Since the mass production of high-fructose corn syrup began in the mid 70s, sweetener consumption in the US has almost doubled, while the population has increased only 40% (see sidebar, next page). Most has come in the form of soft drinks. Dr. Simha comments, “The introduction of sugary beverages has closely paralleled the steep rise in obesity and associated metabolic complications. Most people simply don’t realize the amount of sugar in these beverages. A 20-ounce bottle of regular soda has 17 teaspoons of sugar!” That’s 255 calories, or 13% of the recommended 2,000 calories a typical healthy person engaged in a normal level of physical activity should consume per day from all food and drinks.
According to the Center for Science in the Public Interest (CSPI), Americans consume an average of 577 12-ounce sodas per person per year. That is almost six times the consumption recorded in the 1940s. In CSPI’s 2005 report titled “Liquid Candy: How Soft Drinks Are Harming Americans’ Health,” Michael F. Jacobson, Ph.D. announced that carbonated soft drinks are the single biggest source of calories in the American diet.
Dr. Jacobson explains that soft drinks are a problem not only for what they contain, but for what they push out of the diet. When people consume large amounts of soda, they generally eat less foods that are important sources of vitamins, minerals and dietary fiber.
Soda pop is not the only culprit. Most doctors and scientists have begun using the blanket term “sugary beverages,” which includes sodas, sports beverages, sweetened coffee, the sugary tea that is so common in the Indian diet—and even fruit juice.
How could fruit juice be bad? Fruit juice has the same basic composition as the other beverages on the list: it is mostly sugar and water. According to Dr. Robert Lustig, a pediatric endocrinologist at the University of California at San Francisco, the sugar in fruit juice and the high fructose corn syrup added to sweetened drinks are made up of and broken down by the body into the same two components: glucose and fructose. But juice has more sugar per ounce: eight ounces of juice has about 120 calories, while the same size soda has 100.
Dr. Lustig made the bold claim that sugar is poison in a 2009 lecture he called “Sugar: The Bitter Truth” (on YouTube: bit.ly/sugar-bitter-truth [http://www.bit.ly/sugar-bitter-truth]). This has been the subject of some controversy and only in 2012 began to reach the mainstream media, including a special CNN report by Dr. Sanjay Gupta called “Is Sugar Toxic?” and the comprehensive series “The Weight of the Nation” by HBO Documentaries. In an interview printed by the St. Louis Post-Dispatch on March 22, 2012, Dr. Lustig explained, “Our bodies are not equipped to consume lots of fructose. Glucose, which is found in bread, pasta, rice and potatoes, can be metabolized by all the body’s digestive organs. Fructose can only be metabolized by the liver. If you overwhelm the body with fructose, the liver can’t convert it to energy fast enough. The liver converts it to fat. The goal is to not over-fructosify your liver, but fruit juice does that.”
Dr. Lee A. Evslin, a pediatrician and wellness consultant in Kapaa, Hawaii, expanded on Dr. Lustig’s findings: “There are studies that have shown that when fruit juice is given to what are referred to as the WIC populations (women, infants and children), the obesity rate in most children rose right along with the consumption of the fruit juices.”
Addressing Dr. Lustig’s program for overweight children at UCSF, Dr. Evslin relates: “No liquid sugar. That’s number one. That means no juice, no soda—no carbohydrates without fiber. What they’re talking about is that fruit is high in fructose, but it has fiber in it, and apparently the amount of fiber and the way that fructose is released from its fiber backbone slows it down enough that the body can handle it. It seems to be the rapid absorption of fructose that leads to the liver being overwhelmed.” When you eat the whole fruit, something different happens.
Many of the solid foods people eat today are filled with processed grain products. Dr. Evslin explains: “It is increasingly obvious to anybody looking at the nutrition of the world that everywhere processed food goes, ill-health follows. The shame of our processed food industry is that we’ve narrowed our food choices down to wheat, corn, sugar and soy. We’ve gone from hundreds of varieties of foods that humans were initially exposed to down to these very few, many of them devoid of nutrients because of the depleted soil they’re grown in. We’re giving people fewer and fewer choices.” Think about the typical daily diet: cereal and toast for breakfast, a sandwich for lunch and most likely rice, pasta, potatoes and other starches dominating the dinner plate. That’s a lot of refined carbohydrates and little fiber.
The problem with all those extra calories from the sweetened beverages and starchy meals is that it adds up to far more than the average person engaging in a typical amount of physical activity requires in a day. Where do all those extra calories go? They get converted to fat and stored. Remember what Dr. Simha said happens when fat cells get overstuffed and fat begins to collect in the liver: insulin resistance ensues and type 2 diabetes follows.
The editors of this publication have heard an unfortunate number of Hindus talk in terms of “when” they will get diabetes, not “if.” But people don’t need to get diabetes. If they understood the numerous dire consequences of extra weight and excess sugar in the blood over time and how simple it is to live healthfully, perhaps they would do so.
Dr. Kaufman writes that diabetes is the sixth leading cause of death in the US and that it increases the risk for heart disease sixfold and multiplies the risk of stroke by four. “Diabetes raises cardiac risk because of a process called glycation. Insulin is not required for glucose to enter the cells of the nervous system, including the brain; nor is it needed to allow glucose into red blood cells or into the endothelial cells that line the blood vessels. When too much sugar is circulating in the blood, some of the excess attaches to proteins and molecules in the red blood cells and endothelial cells—this is glycation. The destructive effects of glycation are similar to what happens to fruit as it ripens: first it becomes sweeter and sweeter, then at some point it begins to deteriorate and rot.
“Chronic high blood sugar causes inflammation in the large blood vessels of the heart and brain. Glycation swells the endothelial cells that line the blood vessels. Over time, blood flow to vital organs becomes impaired.” In addition to bringing about heart attacks and strokes, in the US these vascular effects of diabetes annually cause 24,000 people to go blind, 28,000 to end up in kidney failure and 82,000 to require an amputation, losing a toe, a foot or even a leg.
Daily life with diabetes is no walk in the park. “Diabetes never takes a vacation and never gives anyone a break. By the time one shot is finished or one pill is taken, it’s time to prepare for the next. When one blood test is completed, the next one must be anticipated. Each meal or snack requires thought. Some diseases are worse than diabetes. But none requires such a complex balancing act, where patients must do so much themselves. When you’re diagnosed with diabetes, the disease infiltrates every moment and clouds the future,” laments Dr. Kaufman.
The economic costs of diabetes are nothing short of phenomenal. The ADA reports that people with diabetes, on average, have medical expenses 2.3 times higher than those without diabetes and that approximately one in ten health care dollars can be attributed to the disease. The US spends an estimated $2 trillion on health care every year. Do the math.
What can you do?
“The most important thing is to avoid weight gain,” Dr. Simha offers. Studies have concluded that weight reduction not only decreases risk of diabetes dramatically but is more effective than medication for type 2 diabetics, and should thus be the focus of intervention.
“One should be especially mindful of the lower cutoffs for ideal body weight in Asians,” Dr. Simha adds. What he is referring to is the Body Mass Index (BMI), an estimate of body fat composition calculated by dividing weight (kg) by the square of height (m2), and the recent findings that Asians develop diabetes at lower ranges of BMI than other populations. Currently a BMI of 30 kg/m2 or higher is considered the definition of obesity. An August 2011 article in Diabetes Care reads, “For the equivalent incidence rate of diabetes at a BMI of 30 kg/m2 in white subjects, the BMI cutoff value was 24 kg/m2 in South Asian, 25 kg/m2 in Chinese, and 26 kg/m2 in black subjects.” To find out your BMI, enter your height and weight into the tool at bit.ly/mayo-bmi [http://www.bit.ly/mayo-bmi].
Dr. Evslin offers this simple dietary program for a healthy weight: “No liquid sugar; no carbohydrates without fiber.” That means no sodas, juices, sweetened tea or coffee, white rice and white flour (the processing has removed the fiber) and no packaged foods, which are mostly composed of refined corn and wheat. “Returning to real, unsweetened foods, trying to get five to nine servings of fruits and vegetables a day is important,” he advises. The American Heart Association recommends limiting the daily amount of added sugars to no more than 100 calories or six teaspoons of sugar for women and 150 calories or nine teaspoons of sugar for men.
Overall carbohydrate consumption seems to be a problem for a lot of vegetarians. “An American vegetarian frequently eats a lot of bread and pastas. That’s because they’re easy to get. So they can be quite heavy because they’re not eating as many fruits and vegetables as they are bready substances,” avers Dr. Evslin. This applies to the diet our Hindu college students are exposed to in the US; and at home in the West or in India the same can be said about the ratio of rice and rotis to non-starchy vegetables.
While it can’t result in a significant amount of weight loss on its own, regular physical exercise plays a crucial role in metabolism, allowing glucose into cells without insulin. Dr. Simha notes that it helps not only in diabetes prevention but promotion of overall health, adding that the current recommendations are to get at least 150 minutes of aerobic exercise per week (30 minutes five days a week) plus two sessions of resistance/weight training per week. And, he counsels, “It is important to emphasize the intensity of exercise—a leisurely stroll through the park is unlikely to accrue much metabolic benefit.”
What about prediabetes? When asked if those diagnosed with this condition should behave any differently than those with diabetes, Dr. Simha was firm: “No, they should be just as diligent, if not more.” In all circumstances, whether you have prediabetes or diabetes, speaking with your doctor for advice is crucial. But doctors agree that prediabetes will undoubtedly turn into diabetes if no diet and lifestyle changes are made, and that’s a transition that nobody should take lightly.
While individual choice is crucial in the maintenance of good health, there is more to the picture—governmental policies, farm subsidies, food marketing trends and regulations and the habits of billions of people. Dr. Kaufman shares, “We can’t simply blame diabesity on gluttony and laziness. Nor can we assume that the sole solution is individual change. Listening to my young patients talk about their lives, I become angry at a society that doesn’t seem to care, at an economic structure that makes it cheaper to eat fries than fruit, and at the food industry and the mass media luring children to consume what should not be consumed.”
Why Our Food Is Making Us Fat
An excerpt of the exposé by Jacques Peretti printed in the June 11, 2012, edition of The Guardian. The full article may be viewed at bit.ly/peretti-sugar [http://www.bit.ly/peretti-sugar].
THE STORY BEGINS IN 1971. RICHARD NIXON WAS FACING RE-ELECTION. The Vietnam war was threatening his popularity at home, but just as big an issue with voters was the soaring cost of food. If Nixon was to survive, he needed food prices to go down, and that required getting a very powerful lobby on board—the farmers. Nixon appointed Earl Butz, an academic from the farming heartland of Indiana, to broker a compromise. Butz, an agriculture expert, had a radical plan that would transform the food we eat, and in doing so, the shape of the human race.
Butz pushed farmers into a new, industrial scale of production, and into farming one crop in particular: corn. Corn became the engine for the massive surge in the quantities of cheaper food being supplied to American supermarkets: everything from cereals, to biscuits and flour found new uses for corn. As a result of Butz’s free-market reforms, American farmers, almost overnight, went from parochial small-holders to multimillionaire businessmen with a global market.
By the mid-70s, there was a surplus of corn. Butz flew to Japan to look into a scientific innovation that would change everything: the mass development of high fructose corn syrup (HFCS), or glucose-fructose syrup as it’s often referred to in the UK, a highly sweet, gloppy syrup, produced from surplus corn, that was also incredibly cheap. HFCS had been discovered in the 50s, but it was only in the 70s that a process had been found to harness it for mass production. HFCS was soon pumped into every conceivable food: pizzas, coleslaw, meat. It provided that “just baked” sheen on bread and cakes, made everything sweeter, and extended shelf life from days to years. A silent revolution of the amount of sugar that was going into our bodies was taking place.
There was one product in particular that it had a dramatic effect on—soft drinks. Hank Cardello, the former head of marketing at Coca-Cola, tells me that in 1984, Coke in the US swapped from sugar to HFCS (in the UK, it continued to use sugar). As a market leader, Coke’s decision sent a message of endorsement to the rest of the industry, which quickly followed suit. There was “no downside” to HFCS, Cardello says. It was two-thirds the price of sugar, and even the risk of messing with the taste was a risk worth taking when you looked at the margin, especially as there were no apparent health risks. At that time, “obesity wasn’t even on the radar,” says Cardello.
But another health issue was on the radar: heart disease, and in the mid-70s, a fierce debate was raging behind the closed doors of academia over what was causing it. An American nutritionist called Ancel Keys blamed fat, while a British researcher at the University of London, Professor John Yudkin, blamed sugar. But Yudkin’s work was rubbished by what many, including Professor Robert Lustig, one of the world’s leading endocrinologists, believe was a concerted campaign to discredit Yudkin. Much of the criticism came from fellow academics, whose research was aligning far more closely with the direction the food industry was intending to take. Yudkin’s colleague at the time, Dr. Richard Bruckdorfer at UCL says: “There was a huge lobby from [the food] industry, particularly from the sugar industry, and Yudkin complained bitterly that they were subverting some of his ideas.” Yudkin was, Lustig says simply, “thrown under the bus,” because there was a huge financial gain to be made by fingering fat, not sugar, as the culprit of heart disease.
The food industry had its eyes on the creation of a new genre of food, something they knew the public would embrace with huge enthusiasm, believing it to be better for their health—“low fat.” It promised an immense business opportunity forged from the potential disaster of heart disease. But, says Lustig, there was a problem. “When you take the fat out of a recipe, food tastes like cardboard, and you need to replace it with something—that something being sugar.”
Overnight, new products arrived on the shelves that seemed too good to be true. Low-fat yoghurts, spreads, even desserts and biscuits. All with the fat taken out, and replaced with sugar. Britain was one of the most enthusiastic adopters of what food writer Gary Taubes, author of Why We Get Fat, calls “the low-fat dogma,” with sales rocketing.
By the mid-80s, health experts such as Professor Philip James, a world-renowned British scientist who was one of the first to identify obesity as an issue, were noticing that people were getting fatter and no one could explain why. The food industry was keen to point out that individuals must be responsible for their own calorie consumption, but even those who exercised and ate low-fat products were gaining weight. In 1966 the proportion of people [in the UK] with a BMI of over 30 (classified as obese) was just 1.2% for men and 1.8% for women. By 1989 the figures had risen to 10.6% for men and 14.0% for women. And no one was joining the dots between HFCS and fat.
The bitter truth: Dr. Robert Lustig (left) of the University of California at San Francisco postulates that sugar is a poison when consumed in the quantities commonly found today in soft drinks, juices and refined products of all kinds
• • • • • • • • • • • • • • • • • • • •